England’s Men and Women rugby league sides have announced fixtures against France in Toulouse on Saturday June 29, as the French
TECHNOLOGY

Microsoft’s $1.5B check for G42 shows growing US-China rift
As the Gulf region gains growing strategic importance for the tech war between the U.S. and China, Microsoft makes a

Big Tech’s ad transparency tools are still woeful, Mozilla research report finds
Efforts by tech giants to be more transparent about the ads they run are — at very best — still
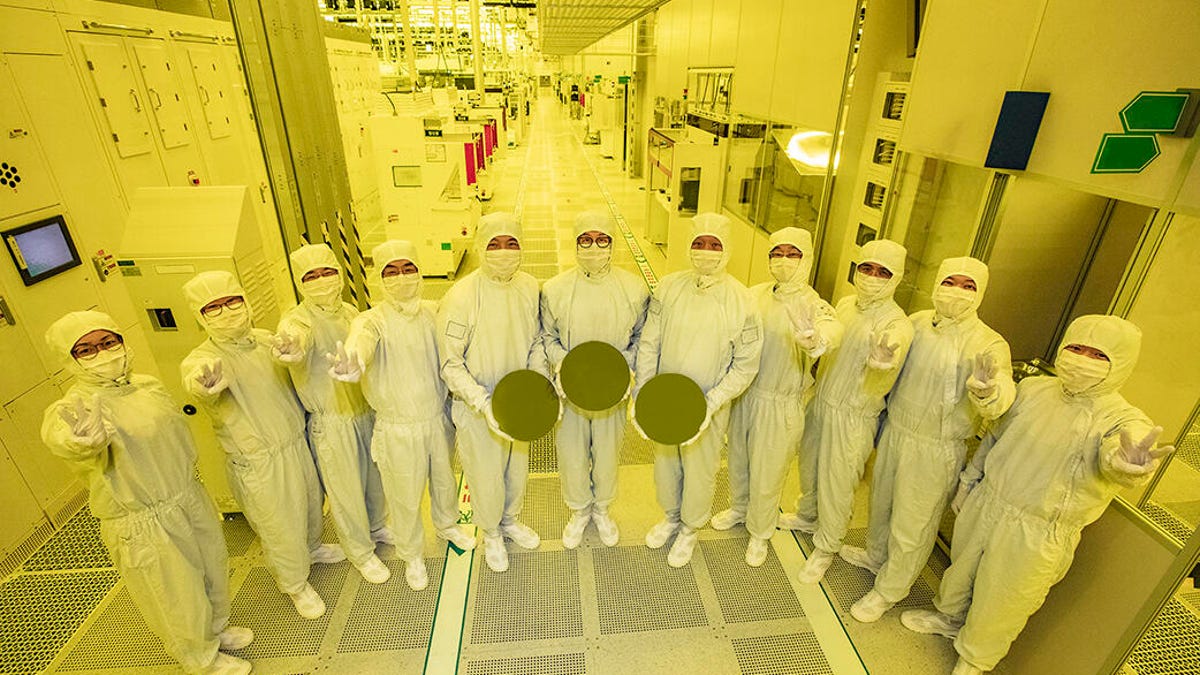
Samsung awarded $6.4 billion by U.S. under CHIPS Act to boost chip production
The U.S. government will give Samsung up to $6.4 billion in direct funding to boost its chip production in Texas,

Tesla layoffs hit high performers, some departments slashed, sources say
Tesla management told employees Monday that the recent layoffs — which gutted some departments by 20% and even hit high

Samsung retakes top phone sales spot from Apple as a third phone maker gains on them both
June Wan/ZDNET According to IDC, Samsung has overtaken Apple as the global leader in smartphone sales. (It was only three
World

‘Mama we’re dying’: Only able to hear her kids in Gaza in their final days | Israel War on Gaza
Bethlehem, occupied West Bank – Hanan al-Qeeq sits next to a hospital bed in Beit Jala Hospital, her sad, pale














