Jason Kelce knows how the rumors fly, and he’s shutting this one down before it gets its wings. After a
TECHNOLOGY

Dripos raises $11M Series A to replace Square, Toast and 8 other pieces of software
Small coffee shops that relied on foot traffic were thrown for a loop when the global pandemic kept people in

Microsoft is now showing ads in Windows 11’s Start menu. Here’s how to block them
NurPhoto/Getty Images Microsoft has rolled out a new way to further mismanage the Windows 11 Start menu: displaying ads in

UK probes Amazon and Microsoft over AI partnerships with Mistral, Anthropic, and Inflection
The U.K.’s Competition and Markets Authority (CMA) is launching preliminary enquiries into whether the close-knit tie-ups and hiring practices involving

Apple Vision Pro FAQ: Price, features, hands-on insights, and everything you need to know
Jason Hiner/ZDNET An Apple AR/VR headset — rumored for more than six years — finally became available this year. Eight
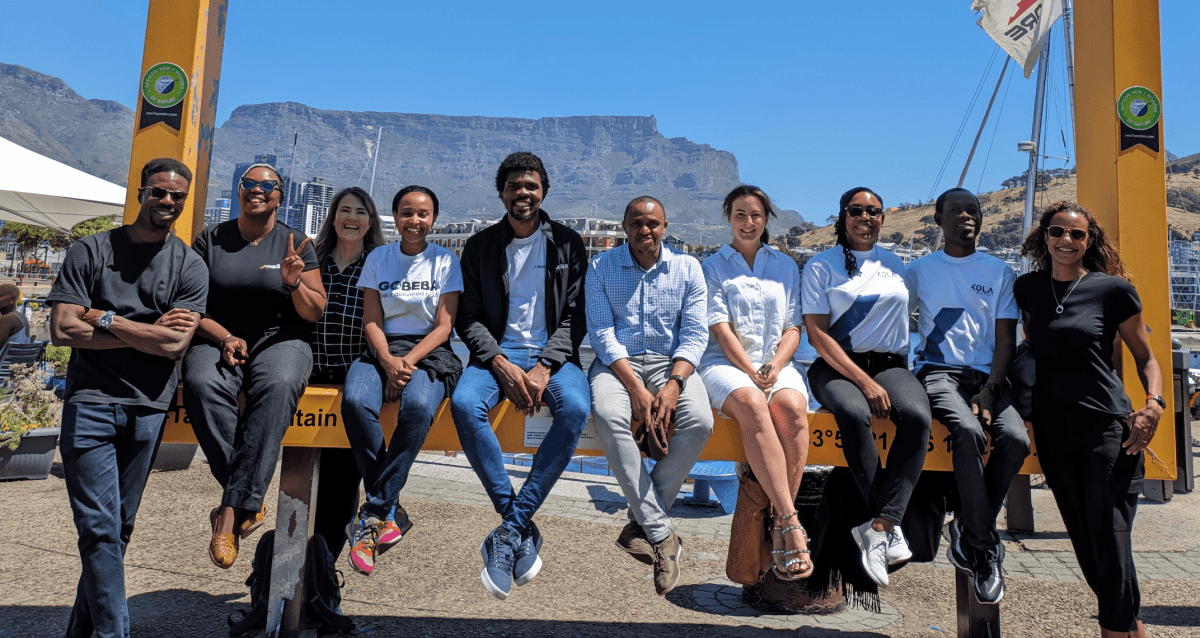
Madica, a program by Flourish Ventures, steps up pre-seed investing in Africa
Madica, an investment program launched by US-based investor Flourish Ventures to back pre-seed startups in Africa, plans to invest in
World

About 282 million people faced acute hunger last year: UN-led report | Hunger News
Food insecurity worsened around the world in 2023, with about 282 million people suffering from acute hunger due to conflicts,














